A flu plan in the health sector
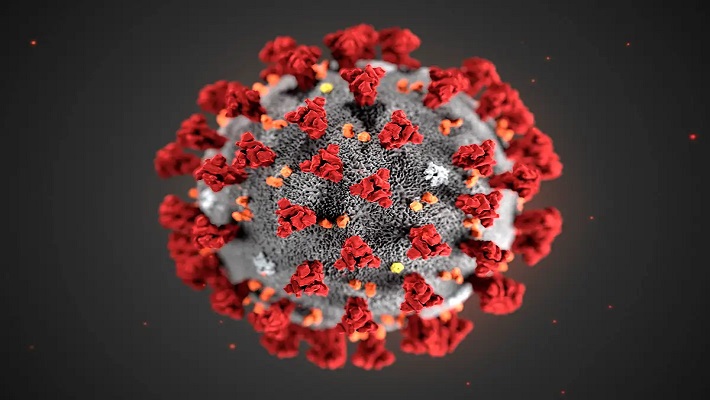
Diseases have often been the plight of humans in every century; it disrupts the norms of human life and disarms the system of governments through public health wars. To tackle infection breakouts, it takes prevention, detection, response and other related schemes in definitive deployment. 1.4 million people have died globally from COVID-19 disease this year.
The Nigerian populace perception of the outbreak of COVID-19 is a measure of surprise and contentious analysis of its spread and arguable cures. The Nigerian President, Muhammadu Buhari in an address to the nation on COVID-19 said ‘I will start by commending you all for the resilience and patriotism that you have shown in our collective fight against the biggest health challenge of our generation.’
A challenge for 774 local government areas and a population barely captured in the last population census after 2006. The spread of the COVID-19 among Nigerians is difficult to trace and may be impossible to diagnose by primary health caregivers at various localities.
“We are at the beginning in Africa”; the Executive Director, Dr Mike Ryan of the World Health Emergencies Programme, informed the world in April 2020.
‘Persons of Interest’- air travellers had arrived in Nigeria from different parts of the world with unverified exposure status as it relates to COVID-19. Unreported self-isolation trend was building up and contact tracing to neighbourhoods and communities was not yielding much result.
The Presidential Task Force (PTF) Chairman, Boss Mustafa had in June 2020 stated that 18 local government areas were responsible for more than 60 percent of COVID-19 cases and the need for a “precision lockdown” was a necessity as the virus was spreading. A pandemic had been localised, an epidemic in the territory and an outbreak shared among loved ones.
More than just a little Flu
Governments around the world had debated on what needs to be done if a disease were to ever spread around the world. Most advanced preparedness and planning structures had been discussed backed by untenable commitments.
The takeaway proclamations from many organised conferences were not helping as the loss of people to COVID-19 trailed on. Jair Bolsonaro, Brazil President, dismissed COVID-19 as a “little flu,” with no severe implications. President Donald Trump declared it is “a badge of honour” that the US has the world’s highest number of confirmed COVID-19 infections.
For States like Kogi, Kano, Jigawa, Cross River and Oyo in Nigeria the issues of infection, testing, contact tracing and tracking of health resources meted into a crisis and systemic arguments on if responses should be localised within the States of the Federation?
The revolving argument by the Kogi government insisting that the Nigerian Centre for Disease Control (NCDC) alongside the Federal government ‘planned to sneak’ cases to its case list and no virus case existed in the State.
‘Mysterious deaths’ had hit Jigawa and Kano State, Nigeria but it was difficult to carry out postmortem due to religious standings on the cause of death; and more political loggerheads to managing COVID-19 was taking place. Many health centres were introduced into debates on the reasonable or recognisable cause of death within their province.
Also, discussions on the infectious disease bill did spring up as the lockdown across Nigeria did swing from one phase to a revised phase. The bill as sponsored by the National Assembly Speaker Femi Gbajabimila suggested that a medical arrest can be made in the interest of the public and also may have subjected the role of Governors to a passive position in the event of an emergency. Nigeria’s Governors Forum criticised the bill as one that left stakeholders out including the chance to contribute to its formulation.
An attempt to decipher the politics and pandemic wars produced only poor results, as propaganda got the best of public health preparedness that could have been available. As death from the pandemic turned the corner, so also was the fund against the epidemic reallocated to other government use exposing the vulnerable public health care systems to fend or collapse.
Dealing with sources of infection
The three tiers of government – Federal, State and Local government had been situated to provide a decentralised health service to Nigerians in various capacities. The health territory hospitals (also known as teaching hospitals) are mainly funded by the Federal Government with a strong outlook to cater for complex and specialised cases from citizens; the General hospitals are backed by State Government with allocations from the federal government and tax from within the States to cater for its residents; the primary health care centres (also called community hospitals by locals) was designed to be tied to local government funding for its operations but they need adequate resources to stand a chance against any outbreak.
The primary health care (PHC) centres deal with frequent and controllable health concerns of a community within their localities from malaria, typhoid, polio, ante-natal but in exceptional cases also had to deal with emerging episodes from localised outbreaks from air and water pollution with an unknown set of causes, or manner of causation (etiology).
Every community shares the resource of air and water; when these resources are contaminated, they often lead to a communal outbreak. Air infection that results in ‘Acute Respiratory Disease (ARD)’ are the leading causes of infectious disease morbidity and mortality in the world…’ according to the World Health Organisation 2007 findings on Epidemic and Pandemic alert and response report. In some instances, the health care centres have to deal with a breakout of water contamination from abattoirs.
According to the Nigeria Health Watch, unsanitary abattoirs are ‘sources of infectious disease that may go unreported’ as the World health organisation estimates that 91 million people fall ill every year due to foodborne diseases in Africa.
The Abia State Commissioner for Agriculture, Ikechi Mgboji, related concern on public health as it relates to infection that is naturally transmissible from vertebrate animals to humans (zoonoses) ‘… any cow offered for public consumption is usually examined by veterinary doctors… two of such cows, when killed, were found to have Bovine Tuberculosis. So, we decided to alert people who eat beef to stop eating the lungs of cows for now. But they may eat the flesh.’
A strange epidemic left 15 people dead in Benue State with symptoms that lasted 48 hours before their demise as the Minister of Health confirmed it was neither Ebola nor COVID-19.
Underfunding of Primary Health Care is a faceoff with death
Combatting a disease can take a lifetime, preparing to curb the spread of a disease takes the strategic brilliance of a government committed to keeping its citizens alive. The sacrificial insight of Doctor Stella Adadevoh saved Nigeria from the widespread Ebola disease in July 2014, despite not having encountered the disease. She had insisted, Patrick Sawyer, patient zero of Ebola travelling into Nigeria should remain in quarantine.
Doctor Adadevoh contracted the disease; contained the spread and protected Nigeria from the death curve. Is the country worth dying for in a public health war with COVID-19?
The National Association of Resident Doctors (NARD) in Nigeria have remained concerned that Doctors are being sent to their death if they have to attend to public health emergencies without the essentially required personal protective equipment; health insurance; delayed payments and poor salaries.
In an exclusive interview, a NARD official, Dr Julian Ojebo said 10 doctors had died in months leading to June 2020 with no insurance; in a related development the Director-General of Nigeria Centre for Disease Control, NCDC Dr Chikwe Ihekweazu in a nationwide briefing in June confirmed the development “We have had 812 health care workers infected, they are not just numbers, 29 of these work for NCDC, they are people I know, they have families, wives and children”.
An insight by Dr. Abubakar Musa Yakubu of family medicine, Muritala Mohammed teaching hospital said ‘…we had no idea what we were dealing with… and so there was fear and panic’. The underfunding of primary health care centers is a faceoff with the threat of death for doctors, patients and health workers alike.
According to WHO Director-General Tedros Adhanom Ghebreyesus, “No country, hospital or clinic can keep its patients safe unless it keeps its health workers safe.”
Almost nothing is known about how doctors working as first responders are keeping safe from COVID-19.
Local governments and health boards don’t have much say on how much money it will take to run a primary health care centre. The State governments hold the finances that keep Local government barely sufficiently alive in its endeavours. The local governments in Nigeria depend on a favourable outlook from the State Governors to be considered for reasonable funding and be prioritised during allocations.
The Oyo State, Executive Secretary, Primary Health Care Board, Doctor Muyideen Babatunde Olatunji explains “we have been able to convince the administration of Governor Seyi Makinde that there is nothing that can be done if primary health care is not funded adequately well.”
He added, “I am convinced to strengthen the institution and provide a legal framework that 7.5 percent of the total allocation to Local government should be given to primary health care service and this can run up to 15 percent as it awaits the assent of the governor.”
Executive Director/CEO, National Primary Health Care Development Agency, Dr Faisal Shuaib in a directive stated that ‘Primary Health Care Centres (PHCs) remains open throughout the country under routine services like immunisation, growth monitoring, antenatal care, childbirth during COVID-19.’
Funding primary health care appears to take on the positive pronouncement among State Governors; the divergent strategy on how much responsibility can be undertaken and should be undertaken continues to provide varying results in primary health care.
In 2005, the arrangement to have public-private partnership (PPP) to improve the quality of health service made good sense; funding for reasons ranging from profits or nonprofits; facility provision, corporate social responsibility, health reforms and political arrangements.
According to National Policy on Public and Private Partnership for Health in Nigeria “public-private partnership” is a collaborative relationship aimed at harnessing (and optimising the use of all available resources in efficient, affordable, accessible, equitable and sustainable health care for all people in Nigeria. The PPP improved responses to communal outbreak, maternal mortality, polio vaccination and health monitoring required care.
Responsiveness of Governors
The Borno State Governor, Professor Babagana Zulum, had taken the trail to improve primary health care allocation to 20 percent in the revised budget to healthcare which had earlier been at eight percent for 2020. Zulum indicated a bill for the establishment of Borno State Contributory Health Management Agency was underway and also keyed into public-private partnerships for health care with international organisations.
The Oyo State Governor, Seyi Makinde pivoted the plans to establish Infectious Disease Centre, Saki (Saki Specialist Hospital) from a COVID-19 recovery centre to 100-bed specialist long term health service hospital. Equipment at the facility upgraded within the 3 months cost up to 250 million naira. This is one of the indicators that responsiveness to health care service is urgent and combined with responsible planning new strides can be attained.
The Abia State information commissioner, John Okiyi, says that 722 primary healthcare centres have been linked to connect to a telehealth centre in a move to allow medical doctors to attend to patients using virtual connections. Okiyi says ‘PHC managers can review cases that are ordinarily beyond their scope and then stabilise a patient with the intent to refer to a secondary or tertiary health facility’.
The responsiveness of governors to the plight caused by COVID-19 in the local and state health sector continues to vary. The proposed budget 2021 and line of action by many state administrators shows that they lack the devotion to invest more resources against emergencies in the health sector.
In Edo State, Governor Godwin Obaseki presented a 2021 budget of 153.4 billion naira as the health sector received an allocation of 10.3 billion naira. Jigawa Governor, Muhammad Badaru presented 156 billion naira budget for 2021 which represents an increase of 29 percent; the health allocation is set at 12.24 billion naira. The Kano Governor, Abdullahi Ganduje has allocated 25 billion naira out of the 147.9 billion naira financial plan for the state.
Approved budgets in Nigeria have often failed to meet many performance indexes and sometimes undergo review and reallocation thereby positioning the health sector in a constant state of emergency.
Many health metrics of Nigeria states for 2021 is devoid of an emergency plan and the 2021 budgetary allocation of Governors have undermined the role of improved health outlook signalling the treatment of emergencies with a flu plan.
As Nigeria deals with the second recession in five years, the mainstay of survival which often lies with the good health of her citizens is bowing out to socio-economic and political machinations of bad choices.
Kano State Governor, Abdullahi Ganduje has presented N147.9 billion as its proposed budget for 2021 fiscal year before the Kano State House of Assembly.
- A breakdown of the budget showed that the Education sector has over N37 Billion representing 25 percent of the total budget while the health care delivery service has over N25 Billion representing 17 percent of the total budget.
The amount comprises N380.21 billion for recurrent expenditure and N132 billion for capital projects. There is also N35.03 billion Basic Health Provision Fund, which includes funds for managing emergencies and infectious diseases such as the COVID-19.
On average, the amount translates to about N2, 735 per Nigerian, given the country’s population of about 200 million people.
Femi D. Amele is an award winning journalist. He is best known for political broadcasts on Nigeria Info, Abuja. He is a fellow at Nigeria Health Watch.
We have recently deactivated our website's comment provider in favour of other channels of distribution and commentary. We encourage you to join the conversation on our stories via our Facebook, Twitter and other social media pages.
More from Peoples Gazette

Politics
Katsina youths pledge to deliver over 2 million votes to Atiku
“Katsina State is Atiku’s political base because it is his second home.”

Sport
Iheanacho, Ndidi secure Premier League promotion with Leicester City
Leicester City have now secured one of the two automatic promotion tickets to the Premier League.

Economy
BDC operators warn against naira speculation, hoarding
He added that ABCON will upgrade technology in its quest to help in the fight against the sabotage of CBN’s reforms.

Economy
Tinubu taps Jim Ovia to lead Nigerian education loan fund
The prominent Nigerian banker was appointed on Friday.

Heading 4
Liverpool agree compensation with Feyenoord to appoint Arne Slot as new manager
Liverpool had initially shown interest in former player and Bayer Leverkusen manager Xabi Alonso.

Agriculture
Taraba govt. set to distribute first set of tractors to farmers
“We have so far received 20 Cabrio and 250 mini high powered tractors that would be distributed to our farmers on May 28.”

NationWide
Jonathan mourns Ayogu Eze
The former president commiserated with the Eze family, his political and professional colleagues in the media.








